For the estimated millions of AIDS patients worldwide who are resistant or are developing resistance to currently available medicines, a discovery by a University of Georgia researcher may offer a new treatment option by targeting a previously elusive enzyme in the complex retrovirus responsible for the devastating disease.
Approximately 40 million people worldwide have the infectious viral disease known as HIV-AIDS. Although the number of drug-resistant patients is extremely difficult to estimate, resistance to AIDS medications is widely viewed as a major global public health problem.
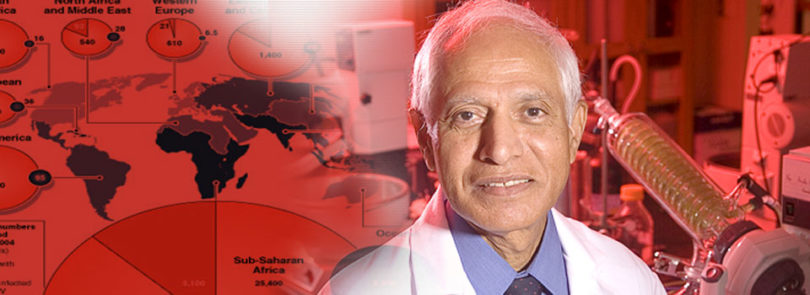
A series of HIV integrase inhibitors discovered by Vasu Nair, Georgia Research Alliance Eminent Scholar in Drug Discovery at the University of Georgia, recently was licensed by Georgia biotechnology company Inhibitex from the University of Georgia Research Foundation. The license included upfront license fees and shares of the company’s common stock, as well as future milestone payments and royalties.
Inhibitex has also agreed to provide significant research funding to support continued research and development activity related to the licensed patents and for drug discovery of new agents to treat patients infected with the hepatitis C virus (HCV). Co-infection by HCV and other viruses is a problem commonly encountered by HIV-AIDS patients.
HIV relies on the activity of three key enzymes to survive and proliferate in the body: reverse transcriptase, protease and integrase. While effective combinations of HIV drugs attack the first two enzymes to stop replication, no fully approved drugs stop the action of the HIV integrase enzyme, the insertion of HIV DNA into human DNA. Nair calls this step in replication “the most devastating” in HIV’s attack on human cells. Because there is no human enzyme counterpart of HIV integrase, it is a particularly significant and attractive disease target in the HIV replication cycle for intervention by therapeutic agents.
In addition, for many AIDS patients, the long-term regimens of anti-HIV drugs prove toxic, and ultimately, their benefits decline. “HIV’s ability to rapidly mutate means that patients usually develop resistance to their treatments over time,” explained Nair.
Now, with HIV integrase inhibitors, “we have a new class of drugs for people that is expected to alleviate some of the problems associated with resistance and provide new treatment options,” said Nair.
“Integrase inhibitors are creating excitement in the pharmaceutical industry, scientific community and for patients,” said Sohail Malik, director of technology commercialization for UGARF. In October, the first integrase inhibitor for drug-resistant AIDS patients was approved by the U.S. Food and Drug Administration (FDA). Its entry into the market is widely considered one of the most important entries into the AIDS pharmaceuticals market in over a decade.
Drug developers have been targeting HIV integrase for years, but without much success. Nair’s own discovery had its beginning in NIH-funded work as far back as 1994, while he was a researcher at the University of Iowa. But, he said of his early research, “those compounds didn’t sufficiently inhibit HIV replication in infected cells.”
It wasn’t until 2002 when he came to the College of Pharmacy at the University of Georgia that he began working on an entirely new class of HIV integrase inhibitors with further NIH research support and had a major breakthrough. All told, Nair, who directs UGA’s interdisciplinary Center for Drug Discovery, has worked for over a decade to bring HIV integrase inhibitors to the point where they could be licensed, an important milestone in the drug discovery, development and approval process.