The National Institutes of Health have awarded, as part of the American Reinvestment and Recovery Act, a two-year,$2 million grant to a UGA genetics researcher and her colleagues for studies on the thymus, the organ in humans that produces disease-fighting T-cells.
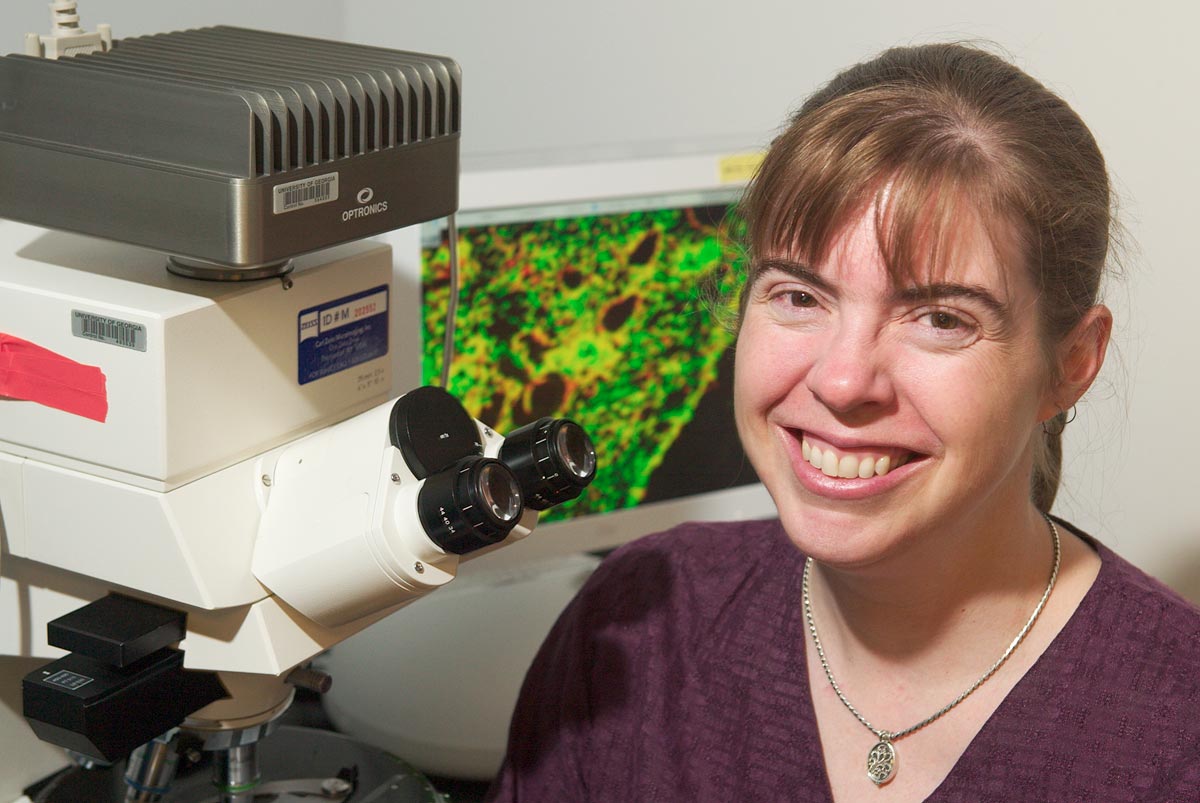
Nancy Manley, a professor of genetics and chair of UGA’s Interdepartmental Biology Group, is the principal investigator on the grant, which will support studies on molecular mechanisms regulating thymic epithelial cells during aging. The new grant supports a collaborative program between UGA, the University of Texas M. D. Anderson Cancer Research Center in Science Park, Texas, and the Center for Stem Cell Research at the University of Edinburgh in Scotland.
Other principal investigators are Ellen Richie, professor of carcinogenesis (Texas) and Clare Blackburn, group leader (Edinburgh).
“This research is an excellent example of how the stimulus money is providing jobs in science and, at the same time, helping unravel new findings that could be important for human health,” Manley said.
The grant will allow her to hire two research scientists, a laboratory technician and a full-time administrator.
While research on the thymus may seem arcane, it is a subject of intense interest and extends and expands work in which Manley has been involved for years.
Last year, Manley’s lab, using the mouse as a biological model, provided the first evidence that a gene may be crucial to maintaining the production of the thymus and its disease-fighting T-cells after an animal’s birth.
The discovery could help scientists find out how to turn the thymus back on so it could produce T-cells long after it normally shuts down most of its function, which, for humans, occurs by early adulthood. If the finding leads to further ways to manipulate the gene, the result could be a new avenue for the body to fight disease more effectively as it ages.
“Such things as infectious diseases, inflammation and heart problems are all related to immune response,” Manley said last year. “You don’t have to think far to see how understanding the effect of this gene could affect the quality of life for older people and others as well.”
The newly funded research will try to discover the actual mechanisms by which the thymus shuts down and how these changes affect immune system function during aging. If and when that mechanism is found, scientists may find a way to turn the organ’s function back on permanently or at specific times in the life of a human or an animal to fight disease or aging. An ultimate payoff might be longer and healthier lives for people.
Until recently, scientists had thought that the thymus after birth was unable to regenerate T-cells because no known regulatory mechanism existed that might allow doctors to “turn back on” the thymus if a person’s T-cells were compromised.
There are now, however, some treatments currently in trials that can transiently rejuvenate the thymus and increase thymic output in humans.
The problem has been, though, that the mechanisms by which all this works are poorly understood, and all current treatments have systemic effects that can cause unacceptable side effects in all but the most seriously ill, who are more willing to tolerate them in exchange for possible benefit.
“So far, the possibility of this working looks very good,” said Manley.
While the mouse model doesn’t precisely mimic human response, it is close enough so that biologists and geneticists can often draw conclusions from mouse trials on how humans will respond.
Under best circumstances, the researchers should know within five to 10 years whether the therapeutic ability to turn back on the production of T-cells is possible.