Muscle aches and pains, whether from stretching, strenuous exercise or just normal wear and tear, can put a crimp in your day, a limp in your step and be an actual pain in the neck. But no matter the severity, stem cells in the skeletal muscles called satellite cells play a key role in repairing the damage.
Without a proper function of satellite cells, as seen in many aged people, muscles are not able to repair damaged parts and can quickly deteriorate, which will eventually cause muscle weakness and fibrosis.
Satellite cells have two states: they either “lurk” or start to turn into muscle. Now, University of Georgia researchers in the Center for Molecular Medicine have found a technology that can control the switch between these two states of satellite cells.
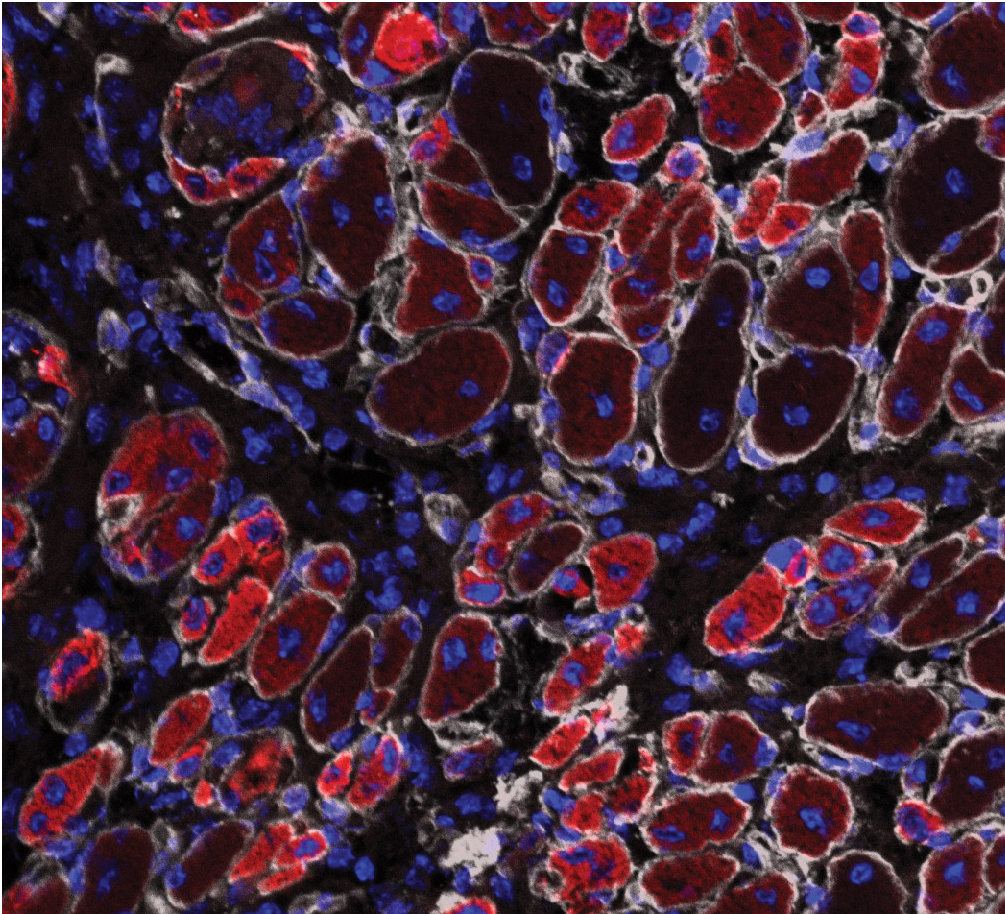
In a healthy muscle, most satellite cells are static non-proliferative cells, lurking and without any overt act. However, when a muscle is damaged, satellite cells start to replicate themselves (proliferation) and turn into muscle cells (differentiation).
“When a muscle is damaged, we can use this technology to turn more satellite cells into muscle cells, which greatly accelerates the muscle repair,” said Hang Yin, assistant professor in the UGA Franklin College of Arts and Sciences department of biochemistry and molecular biology.
For athletes or soldiers in the field, accelerated muscle repair means better recovery of performance and faster deployment; for soldiers or civilians with significant muscle loss, improving satellite cell differentiation may help in the total regeneration of the lost muscle tissue.
For the elderly, better satellite cell function means stronger muscle to support exercise and daily life, which would much improve life quality and reduce health care costs.
The technology centers around how satellite cells sense a low-oxygen state known as hypoxia. If satellite cells sense low oxygen conditions, these stem cells lurk. Conversely, if satellite cells don’t sense the hypoxia, the stem cells start to replicate themselves and turn into muscle.
“We showcased in this study that a small molecular compound called a HIF2a inhibitor can trick satellite cells to sense or not sense hypoxia, and hence control their behaviors,” he said.
A new HIF2a inhibitor has been recently developed and is currently in clinical trials for cancers such as clear cell renal cell carcinoma and glioblastoma. The new study may help to repurpose these types of HIF2a inhibitor drugs for applications to improve muscle repairs and regeneration.
The full study, “Transient HIF2A inhibition promotes satellite cell proliferation and muscle regeneration,” is published in the Journal of Clinical Investigation and is available at https://www.jci.org/articles/view/96208/pdf