The University of Georgia has been ranked among a list of top 10 schools working to solve the coronavirus pandemic by Successful Student. UGA was recognized specifically for research on the development of new vaccines designed to protect against SARS-CoV-2, the virus that causes COVID-19.
Other universities in the top 10 include Harvard University, the University of Oxford and Johns Hopkins University. Successful Student published their rankings online.
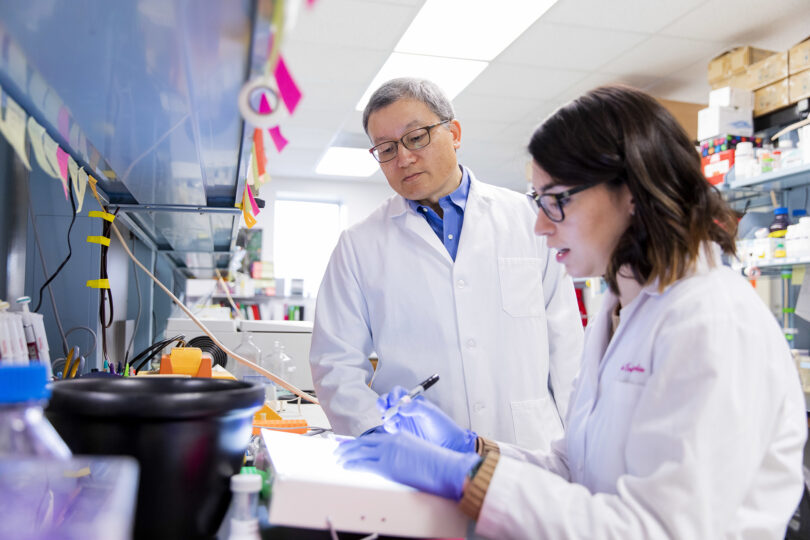
“We have an opportunity now to use our technology to help people. And, at the University of Georgia, we have the people, and we have the facilities. We have been able to quickly mobilize resources to develop this vaccine.” – Biao He
Scientists in laboratories across the university began work on new vaccines and therapeutics from the moment COVID-19 emerged as a global threat.
Biao He, the Fred C. Davison Distinguished University Chair in Veterinary Medicine at UGA, has developed a COVID-19 vaccine candidate that has proven successful in promoting an immune response in early test models.
His vaccine is based on a viral delivery platform containing modified strains of a virus that cause kennel cough in dogs called parainfluenza virus 5, or PIV5. The modified viruses produce proteins found in coronaviruses, specifically the spike proteins that form the “crown” or corona for which they are named. After the vaccine has been administered, cells are infected with the PIV5 virus. The body then begins to mount a defense to the spike proteins produced by the modified virus—ultimately promoting an immunity to infection.
“We have an opportunity now to use our technology to help people,” he said. “And, at the University of Georgia, we have the people, and we have the facilities. We have been able to quickly mobilize resources to develop this vaccine.”
He hopes that the SARS-CoV-2 vaccine will be ready for FDA approval by the end of the year.
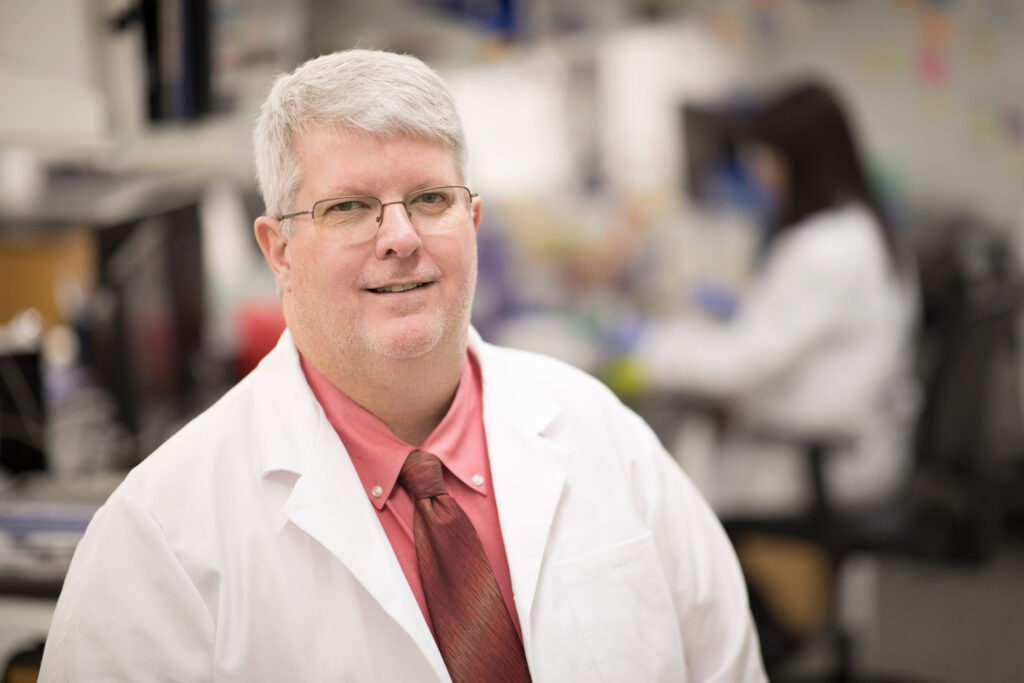
Ted Ross, Georgia Research Alliance Eminent Scholar and director of UGA’s Center for Vaccines and Immunology. (Photo by Peter Frey/UGA)
Scientists in the lab of Ted M. Ross, Georgia Research Alliance Eminent Scholar and director of UGA’s Center for Vaccines and Immunology, are also developing and testing new vaccines and immunotherapies to fight the coronavirus. Ross is working with other researchers in the center to analyze the viral genome and find targets that will prompt the immune system to create protective antibodies.
Ross has spent most of his career studying viruses and developing new vaccines and treatments to combat them, but he is perhaps best known for his efforts to develop a universal influenza vaccine that could protect against all forms of the virus and eliminate the need for seasonal flu shots.
While the lessons learned from his work on influenza and other viruses will inform his work, the coronavirus presents a unique set of challenges.
“Most people already have some immunity to influenza, but nobody has immunity to this coronavirus, which is one reason it has spread so quickly,” Ross said. “The scientific community is hard at work, but there’s still so much we don’t know about this virus, and it will take time to gather quality data.”
The virus that causes COVID-19 is studded on its exterior with “spike proteins,” a key component in its ability to infect human cells. Rob Woods and Parastoo Azadi, both researchers in UGA’s Complex Carbohydrate Research Center, are investigating the proteins and sugars on the surface of the virus with the goal of finding information that could lead to vaccines and therapeutics.
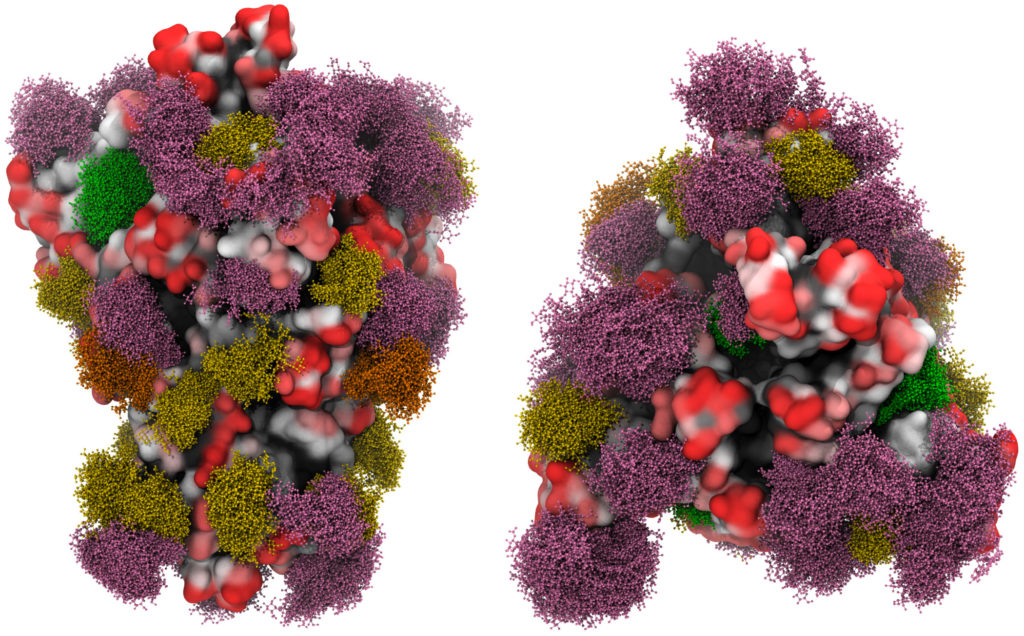
Rob Woods and Parastoo Azadi are investigating the proteins and sugars on the surface of the COVID-19 virus with the goal of finding information that could lead to vaccines and therapeutics. (Submitted photo.)
SARS-CoV-2 spike proteins latch onto cells and force the virus through the cell membrane. The human immune system detects foreign proteins, like the spike protein, by recognizing amino acid sequences that are present, Woods said.
“But if a pathogen puts a sugar on the protein’s surface, it can mask the amino acids,” he said. “One sugar can mask a whole cluster of amino acids so our antibodies can’t see them. Many viruses do this—influenza and hepatitis C, for example.”
The protein is a smooth surface shielded by sugars that move like trees in the wind. That makes it harder for the human immune system to find the target—the protein’s surface.
“I always use the analogy of glycans as trees in the wind. Some of them are floppy, and some of them are more stiff,” Woods said. “We’re looking for ones that we can get under or around.”